The first moments of a newborn’s life are critical, and ensuring their smooth transition to breathing and independent circulation can sometimes require immediate medical intervention. Neonatal resuscitation is a life-saving procedure that equips healthcare professionals, especially nurses, with the skills to respond effectively to emergencies during childbirth. For nursing students, understanding the steps, techniques, and importance of neonatal resuscitation is essential to providing quality care and improving neonatal outcomes.
In this guide, we’ll delve into the fundamentals of neonatal resuscitation, offering clear, concise, and actionable insights tailored to nursing students who aspire to excel in this vital area of healthcare. Neonatal resuscitation is a critical skill required to ensure the survival and health of newborns experiencing difficulty transitioning to life outside the womb. This guide provides an overview of the key principles, steps, and considerations for nursing students.
Definition of Neonatal Resuscitation
Neonatal resuscitation refers to a series of medical interventions aimed at stabilizing newborns who are unable to breathe or maintain adequate circulation immediately after birth. These measures include clearing the airway, providing ventilation, administering oxygen, initiating chest compressions, and, if needed, using medications to ensure the baby’s survival and well-being.
Indications for Neonatal Resuscitation
Neonatal resuscitation is indicated in the following situations:
- Inadequate or Absent Breathing:
- The newborn is not crying or has irregular, weak, or absent respiratory efforts.
- Low Heart Rate:
- Heart rate less than 100 beats per minute despite initial supportive measures.
- Poor Muscle Tone or Color:
- The baby is floppy or has cyanosis (bluish discoloration) indicating inadequate oxygenation.
- Meconium-Stained Amniotic Fluid:
- If the baby is born through meconium-stained fluid and shows signs of distress, resuscitation may be needed.
- Perinatal Complications:
- Prolonged labor, preterm birth, placental abnormalities, or maternal conditions such as diabetes or preeclampsia.
Contraindications for Neonatal Resuscitation
Neonatal resuscitation is generally not performed in the following cases:
- Confirmed Non-Viable Newborns:
- Conditions such as anencephaly or extreme prematurity (<22 weeks gestation), where survival is not expected even with intervention.
- Parental Decisions on Non-Resuscitation:
- In cases where prenatal discussions have led to a decision against resuscitation due to severe anomalies or expected poor prognosis.
- Prolonged Lack of Heartbeat:
- If there is no detectable heartbeat after 10 minutes of effective resuscitation, further efforts may be ceased in alignment with current guidelines and ethical considerations.
Understanding Neonatal Resuscitation
Neonatal resuscitation refers to the emergency measures taken to help newborns initiate effective breathing and circulation immediately after birth. Approximately 10% of newborns require assistance, and about 1% need advanced resuscitative interventions.
Initial Steps of Neonatal Resuscitation
- Assessment of the Newborn:
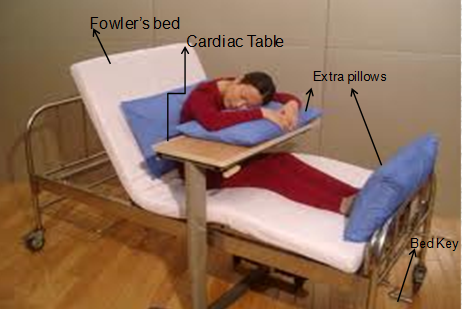
Evaluate the baby’s breathing, heart rate, and color within the first few seconds after delivery. The Apgar score can guide this assessment. - Thermal Management:
Prevent hypothermia by drying the baby, discarding wet towels, and placing the baby in a pre-warmed radiant warmer. Use a polyethylene bag for extremely preterm infants. - Positioning the Airway:
Position the baby’s head in a neutral “sniffing” position to maintain a clear airway. Avoid hyperextension or flexion.
Airway and Breathing Support
- Clearing Secretions:
Suction the mouth and nose only if there is visible obstruction or if the baby has thick secretions and is not breathing effectively. - Positive Pressure Ventilation (PPV):
If the baby is not breathing or has a heart rate <100 bpm, start PPV using a bag-mask device or a T-piece resuscitator. Use 21% oxygen initially for term infants and adjust as needed.
Circulation and Chest Compressions
- Indications for Chest Compressions:
Begin chest compressions if the heart rate remains <60 bpm despite 30 seconds of effective PPV. - Technique:
Use the two-thumb encircling method or two-finger technique, compressing the chest at a depth of one-third its diameter. Coordinate compressions with ventilations at a 3:1 ratio (90 compressions and 30 breaths per minute).
Medications in Neonatal Resuscitation
Administer medications only if the heart rate remains <60 bpm despite adequate ventilation and compressions. Commonly used drugs include:
- Epinephrine: For severe bradycardia or asystole.
- Volume Expanders: For suspected hypovolemia.
Post-Resuscitation Care
- Stabilization:
Monitor vital signs, oxygen saturation, and blood glucose levels. - Ongoing Assessment:
Watch for signs of complications such as hypoxic-ischemic encephalopathy (HIE) or respiratory distress.
Key Considerations for Nursing Students
- Practice Skills: Participate in neonatal resuscitation simulations to gain confidence and proficiency.
- Teamwork: Effective communication and coordination with the resuscitation team are critical.
- Knowledge Updates: Stay informed about the latest guidelines from the Neonatal Resuscitation Program (NRP) and other professional bodies.
Conclusion
Neonatal resuscitation requires prompt and precise actions to save lives. By mastering these skills and adhering to evidence-based guidelines, nursing students can play a vital role in ensuring positive outcomes for newborns in critical situations.
Frequently Asked Questions (FAQs) on Neonatal Resuscitation
What is neonatal resuscitation?
Neonatal resuscitation involves emergency procedures to help a newborn breathe and maintain proper heart function immediately after birth if they are not transitioning well to life outside the womb.
Why is neonatal resuscitation important?
Neonatal resuscitation is vital for preventing brain injury, organ damage, or death in newborns who fail to establish effective breathing or circulation at birth. It ensures a better chance of survival and reduces long-term complications.
Who needs neonatal resuscitation?
Approximately 10% of newborns require some assistance to begin breathing, and about 1% need advanced resuscitative measures. Risk factors include preterm birth, maternal complications, or abnormal fetal monitoring during labor.
What are the first steps in neonatal resuscitation?
The initial steps include:
- Assessing the newborn’s breathing, heart rate, and color.
- Drying and warming the baby to prevent hypothermia.
- Positioning the airway for effective breathing.
- Clearing secretions from the mouth and nose if necessary.
When should positive pressure ventilation (PPV) be started?
PPV should be initiated if the baby:
- Is not breathing or gasping.
- Has a heart rate less than 100 beats per minute after initial steps.
How are chest compressions performed on a newborn?
Chest compressions are performed using either the two-thumb encircling technique or the two-finger method. Compress the chest to one-third its depth at a rate of 90 compressions per minute, paired with 30 breaths (3:1 ratio).
When are medications required in neonatal resuscitation?
Medications are administered if the baby’s heart rate remains below 60 beats per minute despite 30 seconds of effective ventilation and chest compressions. Common medications include epinephrine and volume expanders.
What equipment is used in neonatal resuscitation?
Essential equipment includes:
- Radiant warmer for thermal management.
- Bag-mask device or T-piece resuscitator for ventilation.
- Suction devices for clearing airways.
- Pulse oximeter for oxygen monitoring.
How can nursing students prepare for neonatal resuscitation?
- Participate in hands-on simulations and training programs like the Neonatal Resuscitation Program (NRP).
- Practice effective teamwork and communication during resuscitation scenarios.
- Stay updated on the latest guidelines and evidence-based practices.
What happens after successful neonatal resuscitation?
Post-resuscitation care focuses on stabilizing the baby’s vital signs, monitoring for complications (e.g., hypoxic-ischemic encephalopathy), and providing supportive care such as oxygen therapy or glucose management as needed.
Are there any complications of neonatal resuscitation?
While rare, complications may include:
- Rib fractures or organ injury from chest compressions.
- Airway trauma from improper intubation.
- Hypoxia or acidosis due to delays in initiating effective resuscitation.
How long should resuscitation efforts continue?
Resuscitation efforts may be stopped if there is no heartbeat detected after 10 minutes of continuous and effective resuscitation, as per current guidelines.