Neonatal CPR Cardiopulmonary resuscitation (CPR) is a lifesaving procedure performed to restore breathing and circulation in individuals who have suffered a cardiac or respiratory arrest. Neonatal CPR is a specialized form of this intervention, tailored to meet the unique physiological needs of newborns. Nurses play a crucial role in recognizing the need for CPR and executing it efficiently in neonates.
Definition
Neonatal CPR refers to the emergency medical procedure performed on newborns (infants less than 28 days old) to maintain oxygenation and circulation when their heart or breathing stops or is inadequate.
Indications
- Apnea or gasping respirations.
- Heart rate less than 60 beats per minute despite adequate ventilation with 100% oxygen.
- Signs of severe bradycardia or poor perfusion.
- Persistent cyanosis despite resuscitation efforts.
Contraindications
- Neonates with confirmed fatal anomalies or conditions incompatible with life.
- Presence of a valid do-not-resuscitate (DNR) order.
- Situations where resuscitation efforts would cause undue suffering with no realistic hope of success.
Preparation
- Ensure availability of resuscitation equipment, including a neonatal bag-mask, oxygen source, intubation supplies, and a cardiac monitor.
- Assemble a skilled resuscitation team.
- Maintain a warm environment to prevent neonatal hypothermia.
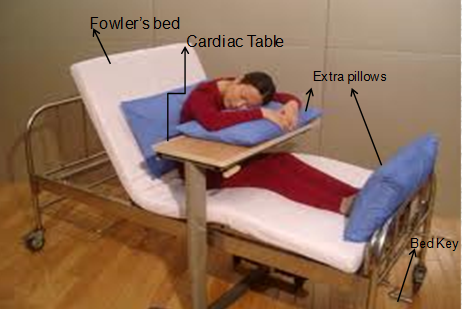
- Position the neonate on a firm surface with the head slightly extended to maintain airway patency.
Procedure
Steps of Neonatal CPR:
- Initial Assessment:
- Assess the neonate for responsiveness, breathing, and heart rate.
- If the neonate is unresponsive or has a heart rate below 100 bpm, initiate resuscitation.
- Airway Management:
- Position the neonate’s head in the sniffing position.
- Clear the airway of secretions using suction if needed.
- Breathing:
- Provide positive pressure ventilation (PPV) using a neonatal bag-mask with 100% oxygen.
- Reassess after 30 seconds; if the heart rate is still below 60 bpm, proceed to chest compressions.
- Chest Compressions:
- Perform compressions using the two-thumb encircling technique or the two-finger technique.
- Compress the lower third of the sternum to a depth of approximately one-third of the anterior-posterior chest diameter.
- Compression-to-Ventilation Ratio:
- Use a ratio of 3 compressions to 1 ventilation (3:1), providing 120 events per minute (90 compressions and 30 breaths).
- Medications:
- Administer epinephrine if the heart rate remains below 60 bpm despite effective CPR.
- Provide volume expanders if hypovolemia is suspected.
Nursing Considerations
- Assessment and Monitoring:
- Continuously monitor the neonate’s heart rate, oxygen saturation, and respiratory status.
- Observe for signs of improvement, such as spontaneous breathing or increased heart rate.
- Team Communication:
- Ensure clear and concise communication within the resuscitation team.
- Document all interventions, including the time and dose of medications administered.
- Equipment Management:
- Ensure all resuscitation equipment is functional and readily available.
- Check oxygen supply and ventilation devices for proper functioning.
- Post-Resuscitation Care:
- Monitor for complications such as hypoglycemia, hypothermia, or metabolic acidosis.
- Transfer the neonate to a higher level of care if needed.
- Parental Support:
- Provide emotional support and clear communication to the parents during and after the procedure.
- Thermal Management:
- Ensure the neonate is kept warm using warm blankets, radiant warmers, or skin-to-skin contact with the mother when possible, while balancing resuscitation needs.
- Hypothermia can worsen neonatal outcomes during and after resuscitation.
- Oxygenation Guidelines:
- Avoid hyperoxia, as excessive oxygen can lead to oxygen toxicity.
- Use pulse oximetry to titrate oxygen delivery and aim for target oxygen saturations according to neonatal resuscitation guidelines (e.g., 60%-65% at 1 minute, increasing to 85%-95% by 10 minutes after birth).
- Family-Centered Care:
- Inform the family about the neonate’s condition with empathy and clarity.
- Allow parents to observe the resuscitation if appropriate, as it can help them understand the efforts made to support their child.
- Debriefing and Education:
- Conduct a debriefing session with the resuscitation team after the event to review performance and identify areas for improvement.
- Offer ongoing training sessions for nurses and staff to maintain proficiency in neonatal CPR.
- Ethical Considerations:
- In cases involving end-of-life decisions or prolonged resuscitation with poor prognosis, involve the healthcare team and family in decision-making while adhering to ethical guidelines.
- Documentation Tips:
- Record precise details, including the time of each intervention, medication administration, and the neonate’s response.
- Use structured formats or templates for comprehensive and clear documentation.
Conclusion
Neonatal CPR is a critical intervention that requires prompt action, precision, and teamwork. Nurses must be well-trained in recognizing the indications for CPR, preparing appropriately, and performing the procedure effectively. Continuous education, skill practice, and adherence to updated guidelines ensure the best possible outcomes for neonates in critical situations.
FAQs
Here are some frequently asked questions (FAQs) about neonatal CPR:
1. What is neonatal CPR? Neonatal CPR is an emergency medical procedure performed on newborns (infants less than 28 days old) to restore breathing and circulation when their heart or breathing has stopped or is inadequate.
2. When is neonatal CPR necessary? Neonatal CPR is indicated in situations such as apnea (absence of breathing), gasping respirations, a heart rate less than 60 beats per minute despite adequate ventilation, or persistent cyanosis (bluish discoloration) despite resuscitation efforts.
3. What are the key steps in performing neonatal CPR? The primary steps include:
- Initial Assessment: Check the neonate’s responsiveness, breathing, and heart rate.
- Airway Management: Position the head to open the airway and clear any secretions.
- Breathing: Provide positive pressure ventilation if the neonate is not breathing adequately.
- Chest Compressions: If the heart rate remains below 60 beats per minute despite ventilation, initiate chest compressions.
- Medication: Administer epinephrine if there’s no improvement after effective CPR.
4. What is the recommended compression-to-ventilation ratio in neonatal CPR? The recommended ratio is 3 compressions to 1 ventilation (3:1), aiming for approximately 120 events per minute (90 compressions and 30 ventilations).
5. Are there any contraindications for neonatal CPR? Contraindications may include neonates with confirmed fatal anomalies or conditions incompatible with life, the presence of a valid do-not-resuscitate (DNR) order, or situations where resuscitation efforts would cause undue suffering with no realistic hope of success.
6. How important is thermal management during neonatal resuscitation? Maintaining the neonate’s body temperature is crucial. Hypothermia can worsen outcomes during and after resuscitation. Use warm blankets, radiant warmers, or skin-to-skin contact with the mother when possible, while balancing resuscitation needs.
7. What role does oxygen play in neonatal resuscitation? Oxygen should be used judiciously. Avoid hyperoxia, as excessive oxygen can lead to oxygen toxicity. Use pulse oximetry to titrate oxygen delivery and aim for target oxygen saturations according to neonatal resuscitation guidelines.
8. How can parents be supported during neonatal resuscitation? Provide emotional support and clear communication to the parents during and after the procedure. Allowing parents to observe the resuscitation, when appropriate, can help them understand the efforts made to support their child.