Imagine facing surgery not with anxiety about a long, painful recovery, but with confidence, knowing you’ve chosen the most advanced and patient-friendly option available. This is the reality of a laparoscopic hysterectomy.
This minimally invasive procedure revolutionizes how we approach uterine surgery. By utilizing small keyhole incisions, a sophisticated camera (laparoscope), and specialized instruments, surgeons can perform this complex procedure with unparalleled precision. The result? It has rapidly become the preferred alternative to traditional open surgery for one powerful reason: it prioritizes your well-being, offering you the incredible benefits of a faster recovery, significantly less pain, and minimal scarring.
If you’re considering this path to better health, you’re in the right place. This guide will illuminate every aspect of the journey – from preparation to recovery – empowering you with the knowledge you need to make a confident and informed decision.
Table of Contents
In the U.S., over 600,000 hysterectomies are performed annually, making it one of the most common surgical procedures for women. Laparoscopic techniques are increasingly the standard of care due to their significant benefits over traditional open surgery. This guide covers everything you need to know—types, benefits, risks, recovery, and FAQs—to help you make an informed decision about your healthcare.
What is a Laparoscopic Hysterectomy?
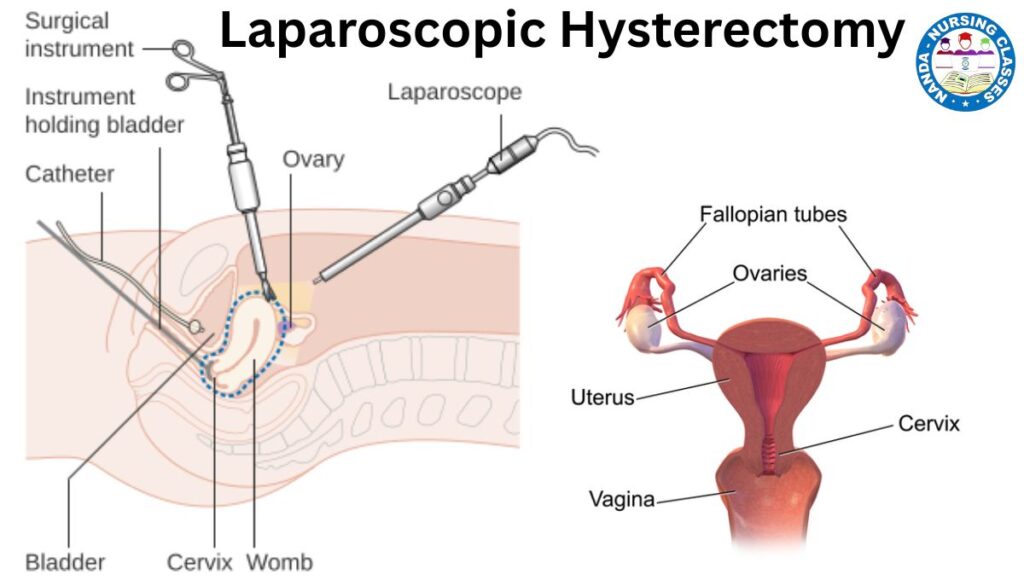
A laparoscopic hysterectomy involves removing the uterus through small abdominal incisions (usually 0.5-1.5 cm) instead of a large open cut. The surgeon uses a laparoscope (a thin tube with a camera) and long, thin instruments to perform the surgery while viewing a high-definition monitor.
Types of Laparoscopic Hysterectomy
- Total Laparoscopic Hysterectomy (TLH) – Removes the entire uterus, including the cervix.
- Laparoscopic Supracervical Hysterectomy (LSH) – Removes only the upper uterus, leaving the cervix.
- Laparoscopically Assisted Vaginal Hysterectomy (LAVH) – Combines laparoscopic and vaginal approaches.
- Robot-Assisted Laparoscopic Hysterectomy – Uses robotic technology (like the da Vinci system) for enhanced precision.
How do you know which type of laparoscopic hysterectomy you will undergo?
Click here to know more about Hysterectomy types
Why is a Laparoscopic Hysterectomy Performed?
Common reasons for this surgery include:
- Uterine fibroids (non-cancerous growths causing pain or bleeding)
- Endometriosis (uterine tissue growing outside the uterus)
- Adenomyosis (thickening of the uterine wall)
- Chronic pelvic pain
- Abnormal uterine bleeding (heavy or irregular periods)
- Gynecologic cancers (uterine, cervical, or ovarian cancer in some cases)
Advantages of Laparoscopic Hysterectomy
Compared to open abdominal hysterectomy, laparoscopic surgery offers:
✅ Smaller incisions (less scarring)
✅ Less post-operative pain
✅ Shorter hospital stay (often same-day or 1-night stay)
✅ Faster recovery (2-4 weeks vs. 6-8 weeks for open surgery)
✅ Lower risk of infection and blood loss
Risks and Complications
While generally safe, possible risks include:
- Bleeding or infection
- Damage to nearby organs (bladder, bowel, blood vessels)
- Blood clots (deep vein thrombosis)
- Conversion to open surgery (if complications arise)
- Anesthesia-related risks
What to Expect: Before, During, and After Surgery
Before Surgery
- Pre-op tests (blood work, imaging, pelvic exam)
- Medication adjustments (stop blood thinners if prescribed)
- Fasting (no food or drink 8-12 hours before)
- Bowel prep (sometimes required)
During Surgery
- Anesthesia: General anesthesia is used.
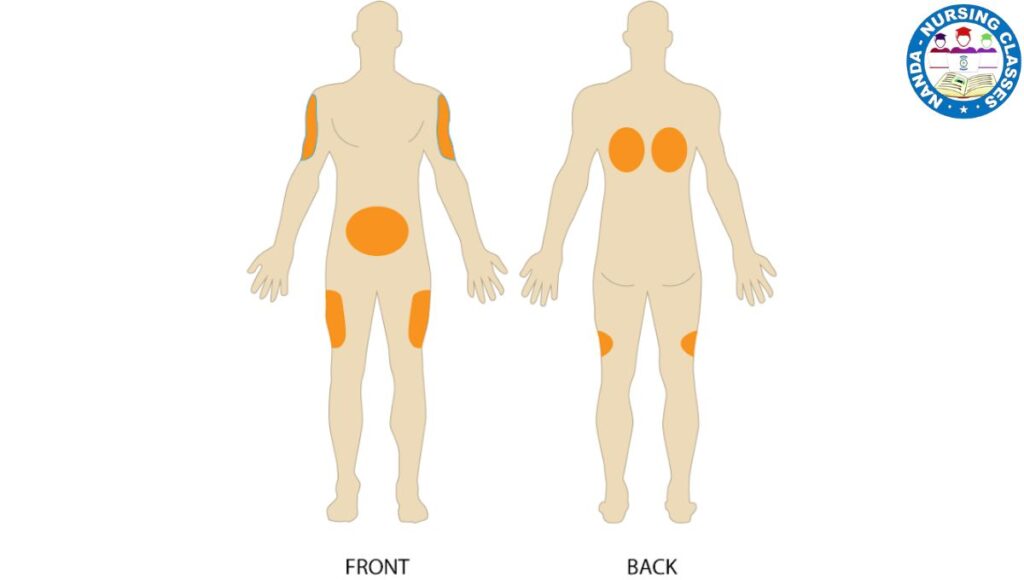
- Incisions: 3-4 small cuts are made in the abdomen.
- Gas inflation: The abdomen is filled with CO₂ gas for better visibility.
- Uterus removal: The surgeon detaches the uterus and removes it through the vagina or in small pieces.
- Closure: Incisions are closed with stitches or surgical glue.
Surgery Duration: 1-3 hours, depending on complexity.
After Surgery (Recovery Timeline)
- Hospital Stay: Usually outpatient or 1-2 days.
- Pain Management: Mild to moderate pain (medications prescribed).
- Activity Restrictions:
- First Week: Light walking, no heavy lifting (>10 lbs).
- 2-4 Weeks: Gradual return to normal activities.
- 6 Weeks: Full recovery (sex, exercise allowed after doctor’s approval).
- Follow-Up: Post-op checkups to monitor healing.
The Step-by-Step Procedure
Phase 1: Preparation
- Anesthesia: You will receive general anesthesia, meaning you will be completely asleep and feel no pain during the surgery.
- Positioning: You will be placed on the operating table in the dorsal lithotomy position (on your back with your legs in stirrups, similar to a Pap smear). This allows the surgeon access to both your abdomen and vagina.
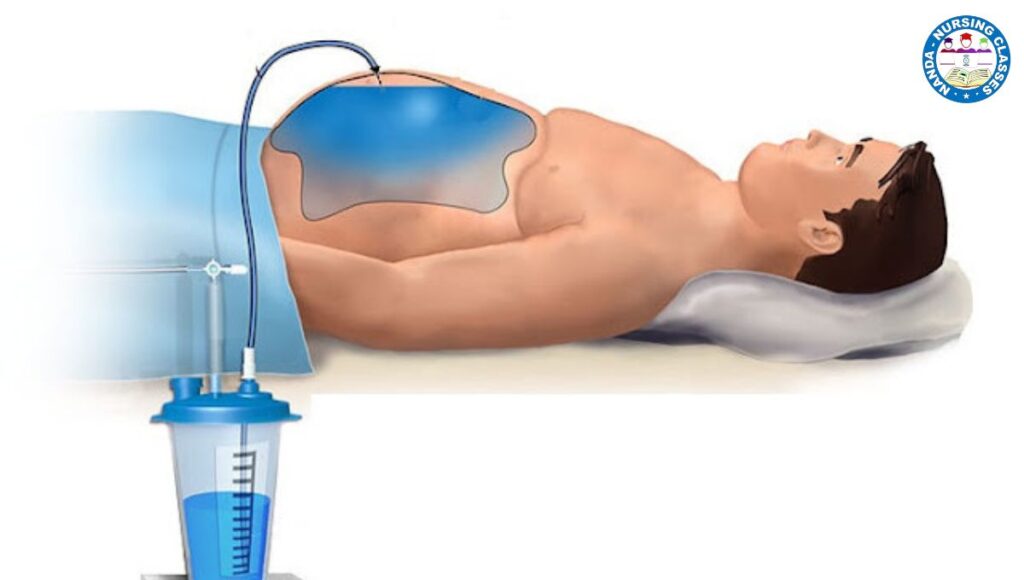
- Urinary Catheter: A thin tube (catheter) is inserted into your bladder to drain urine and keep the bladder empty and out of the way during surgery.
Phase 2: Gaining Access – The Keyhole Incisions
- The surgeon makes a very small incision (usually at the navel) and inserts a needle to fill your abdominal cavity with carbon dioxide gas. This inflates the abdomen, creating a clear working space and moving your intestines away from the uterus, giving the surgeon a better view and more room to operate.
- The laparoscope is then inserted through this incision.
- The surgeon makes 2 to 4 additional small incisions in your lower abdomen. These ports are used to insert specialized long, thin surgical instruments (like scissors, graspers, and cautery devices).
Phase 3: The Surgical Removal
This is the most complex part and involves carefully separating the uterus from the surrounding structures. The surgeon uses the video monitor to guide the instruments.
- Visualization: The laparoscope provides a magnified view of your pelvic organs—uterus, ovaries, fallopian tubes, bladder, and intestines.
- Cutting Connections: The surgeon carefully identifies and cuts the attachments holding the uterus in place:
- Blood Vessels: The uterine artery and other blood vessels are sealed using an energy device that cuts and cauterizes (seals with heat) simultaneously to prevent bleeding.
- Ligaments: The supportive ligaments are divided.
- Ovaries & Tubes: The surgeon will decide whether to remove the ovaries (oophorectomy) and fallopian tubes (salpingectomy) based on the reason for your surgery. If they are healthy, they are often left in place.
- Separating from the Bladder and Bowel: The uterus is carefully separated from the bladder at the front and the rectum (bowel) at the back.
Phase 4: Removing the Uterus
There are two main techniques for removing the uterus once it is free:
- Laparoscopic Supracervical Hysterectomy (LSH): Only the upper part of the uterus is removed. The cervix is left in place. The uterus is cut into small pieces (morcellation) and removed through the small abdominal incisions.
- Total Laparoscopic Hysterectomy (TLH): The entire uterus, including the cervix, is removed. The most common method is to detach it from the top (laparoscopically) and then remove it through the vagina. The top of the vagina (the cuff) is then stitched closed with dissolvable stitches.
Phase 5: Closing Up
- The surgeon checks all areas for any signs of bleeding and ensures all structures are intact.
- The carbon dioxide gas is released from your abdomen.
- The small incisions are closed with a few stitches or surgical glue and covered with small bandages. The vaginal cuff (if the cervix was removed) is closed with dissolvable sutures.
Advantages Over Open Abdominal Hysterectomy
- Smaller Incisions: Less scarring.
- Less Pain: Significantly less post-operative pain.
- Shorter Hospital Stay: Often just one night or sometimes same-day discharge.
- Quicker Recovery: Most return to normal activities in 2-4 weeks instead of 6-8.
- Less Blood Loss: Lower risk of transfusion.
- Lower Risk of Infection: Smaller wounds have a lower risk of infection.
Recovery: What to Expect
- Post-Op: You will wake up with some abdominal cramping and shoulder pain (from the residual CO2 gas, which irritates the diaphragm; it resolves in 24-48 hours).
- At Home: You will be advised to avoid heavy lifting (nothing over 10-15 lbs) and strenuous activity for several weeks. Light walking is encouraged to aid recovery.
- Vaginal Discharge: Some light bleeding or spotting is normal for a few weeks.
- Follow-up: You will have a post-operative appointment to check your incisions and healing progress.
Important Considerations
- Not for Everyone: The procedure may not be suitable for those with very large uteruses (often beyond 12-14 week size), extensive scar tissue (adhesions) from previous surgeries, or certain medical conditions.
- Surgeon Skill: Requires a surgeon with specialized training in advanced laparoscopic techniques.
- Risks: As with any major surgery, risks include infection, bleeding, injury to surrounding organs (bladder, bowel, ureters), blood clots, and complications from anesthesia.
This explanation provides a comprehensive overview. Always discuss your specific case, the type of hysterectomy recommended for you, and all potential risks and benefits with your gynecologist or surgeon.
FAQs About Laparoscopic Hysterectomy
1. How long does it take to recover?
Most women resume light activities in 2-4 weeks and full activities in 6 weeks.
2. Will I go into menopause after a hysterectomy?
Only if the ovaries are removed (oophorectomy). Otherwise, menopause occurs naturally.
3. Can I get a laparoscopic hysterectomy if I have large fibroids?
Yes, but very large fibroids may require open surgery.
4. What are the restrictions after surgery?
- No heavy lifting (>10 lbs) for 4-6 weeks.
- No intercourse for 6 weeks.
- Avoid strenuous exercise until cleared by your doctor.
5. Are there alternatives to a hysterectomy?
Yes, depending on the condition:
- Uterine artery embolization (for fibroids)
- Endometrial ablation (for heavy bleeding)
- Myomectomy (fibroid removal only)
6. Does insurance cover a laparoscopic hysterectomy?
Most U.S. health insurance plans (including Medicare/Medicaid) cover it if medically necessary.
Conclusion
A laparoscopic hysterectomy is a safe, effective, and minimally invasive option for women needing uterus removal. With faster recovery and fewer complications than open surgery, it’s a preferred choice for treating fibroids, endometriosis, and other gynecologic conditions.
If you’re considering this procedure, consult a board-certified gynecologic surgeon to discuss the best approach for your health needs.