A hysterectomy is one of the most common gynecological surgeries performed worldwide, involving the removal of a woman’s uterus. It may also include the removal of surrounding structures such as the cervix, ovaries, and fallopian tubes. Nursing students must understand this procedure thoroughly, as they play a crucial role in preoperative preparation, intraoperative assistance, and postoperative care.
This guide covers types of hysterectomy, indications, complications, preoperative preparation, step-by-step procedure with rationale, contraindications, postoperative care (including tracheostomy care if needed), and FAQs to help nursing students excel in clinical practice.
Content in this Page
What is a Hysterectomy?
A hysterectomy is the surgical removal of the uterus, and sometimes adjacent reproductive organs. It is performed to treat various gynecological conditions, including cancer, chronic pain, and abnormal uterine bleeding.
Types of Hysterectomy
A hysterectomy is the surgical removal of the uterus and may also involve the removal of other reproductive organs. There are several types of hysterectomies, classified based on the extent of tissue removed and the surgical approach used.
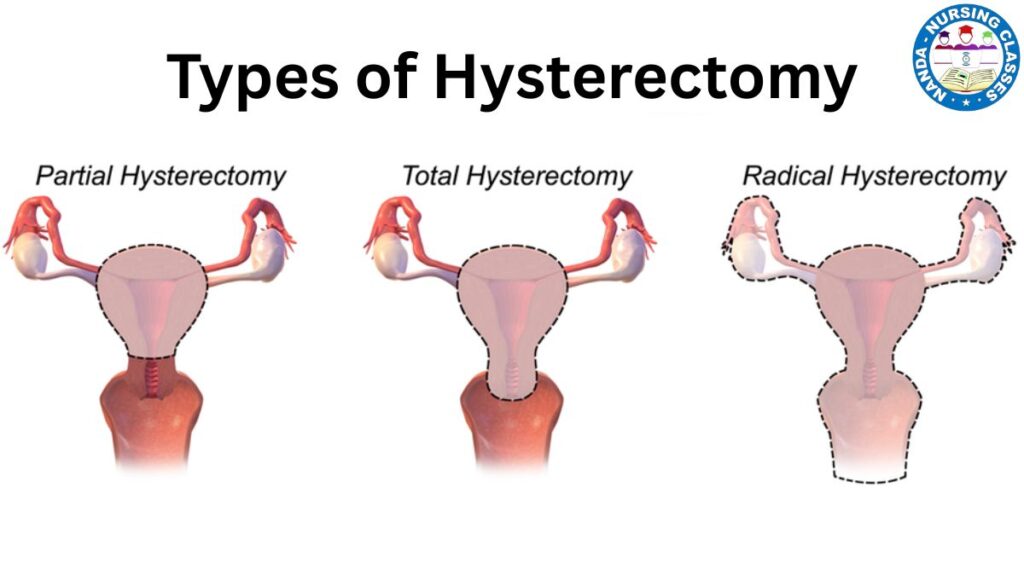
What is a partial hysterectomy ?
Supracervical (Subtotal) Hysterectomy
A supracervical hysterectomy (also called a subtotal or partial hysterectomy) involves removing the upper part of the uterus while leaving the cervix intact. Unlike a total hysterectomy, the cervix and supporting ligaments remain in place.
Total Hysterectomy
A total hysterectomy is a surgical procedure to remove the uterus (womb) and cervix. Depending on the patient’s condition, the surgeon may also remove other structures, such as the fallopian tubes and ovaries (salpingo-oophorectomy).
Radical Hysterectomy
A radical hysterectomy is an extensive surgical procedure primarily used to treat gynecologic cancers, particularly cervical cancer, but sometimes also endometrial cancer or other pelvic malignancies. Unlike a standard total hysterectomy, this surgery involves removing more tissue to ensure complete cancer removal.
Types of Radical Hysterectomy
- Type I (Simple/Total Hysterectomy) – Removes uterus and cervix (not truly radical).
- Type II (Modified Radical Hysterectomy) – Removes uterus, cervix, upper vagina, and some parametrial tissue.
- Type III (Classic Radical Hysterectomy – Wertheim/Meigs procedure) – Removes uterus, cervix, upper vagina, parametrium, and pelvic lymph nodes.
- Type IV (Extended Radical Hysterectomy) – Removes additional vaginal tissue and may include ureter or bladder resection in advanced cases.
Hysterectomy with Bilateral Salpingo-Oophorectomy
A hysterectomy with bilateral salpingo-oophorectomy (BSO) is a surgical procedure that removes:
- Uterus (womb)
- Cervix (unless a supracervical approach is used)
- Both fallopian tubes (salpingectomy)
- Both ovaries (oophorectomy)
This is often referred to as a “total hysterectomy with BSO” and is more extensive than a standard hysterectomy.
Must Read
Surgical Approaches
- Abdominal Hysterectomy (Open surgery via abdominal incision)
- Vaginal Hysterectomy (Removal through the vagina, least invasive)
- Laparoscopic Hysterectomy (Minimally invasive, using small incisions and a camera)
- Robotic-Assisted Hysterectomy (Precision surgery using robotic technology)
Indications for Hysterectomy
- Uterine fibroids (causing pain or heavy bleeding)
- Endometriosis (severe, unresponsive to medication)
- Gynecologic cancers (uterine, cervical, ovarian)
- Chronic pelvic pain (unresponsive to other treatments)
- Uterine prolapse (when the uterus slips into the vaginal canal)
- Abnormal uterine bleeding (not controlled by medication)
- Adenomyosis (thickening of the uterine wall)
Complications of Hysterectomy
- Hemorrhage (excessive bleeding)
- Infection (UTI, wound infection, pelvic abscess)
- Deep Vein Thrombosis (DVT)
- Damage to nearby organs (bladder, bowel, ureters)
- Early menopause (if ovaries are removed)
- Adhesions (scar tissue formation)
- Anesthesia-related risks
What is a laparoscopic hysterectomy
A laparoscopic hysterectomy is a minimally invasive surgical procedure to remove the uterus (and sometimes the cervix, fallopian tubes, and ovaries) using small incisions and a laparoscope (a thin, lighted tube with a camera).
to read more about laparoscopic hysterectomy click here
Preoperative Preparation
Nursing Responsibilities Before Hysterectomy
✅ Patient Education – Explain the procedure, risks, and recovery.
✅ Informed Consent – Ensure the patient understands and signs consent forms.
✅ Medical History & Allergies – Assess for bleeding disorders, prior surgeries.
✅ Lab Tests – CBC, coagulation profile, blood typing, urinalysis.
✅ Bowel Preparation – Some surgeons require bowel cleansing.
✅ NPO Status – No food/water 8-12 hours before surgery.
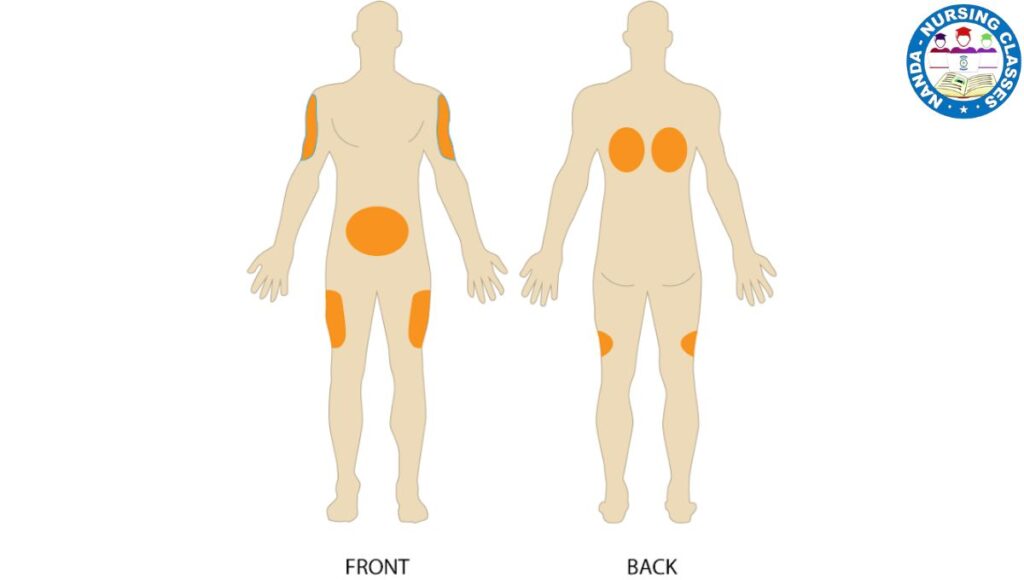
✅ Skin Preparation – Shaving and antiseptic cleaning of the surgical site.
✅ IV Access & Prophylactic Antibiotics – To prevent infection.
Step-by-Step Hysterectomy Procedure with Rationale
1. Anesthesia Administration
- General or regional anesthesia is given to ensure patient comfort.
2. Surgical Approach (Depends on Type)
- Abdominal: Midline/Pfannenstiel incision → uterus removed.
- Vaginal: Uterus detached and removed through the vagina.
- Laparoscopic/Robotic: Small incisions, camera-guided removal.
3. Clamping & Cutting Blood Vessels
- Rationale: Prevents excessive bleeding.
4. Removal of Uterus & Surrounding Structures (if needed)
- Rationale: Treats underlying condition (e.g., cancer, fibroids).
5. Closure of Incisions
- Sutures/Staples for abdominal; absorbable stitches for vaginal.
6. Postoperative Monitoring
- Vital signs, pain management, bleeding assessment.
Contraindications for Hysterectomy
❌ Pregnancy (unless life-threatening condition)
❌ Uncontrolled bleeding disorders
❌ Active pelvic infection (unless emergency)
❌ Patient refusal or unstable medical condition
Postoperative Care & Tracheostomy Care (If Applicable)
Immediate Post-Op Nursing Care
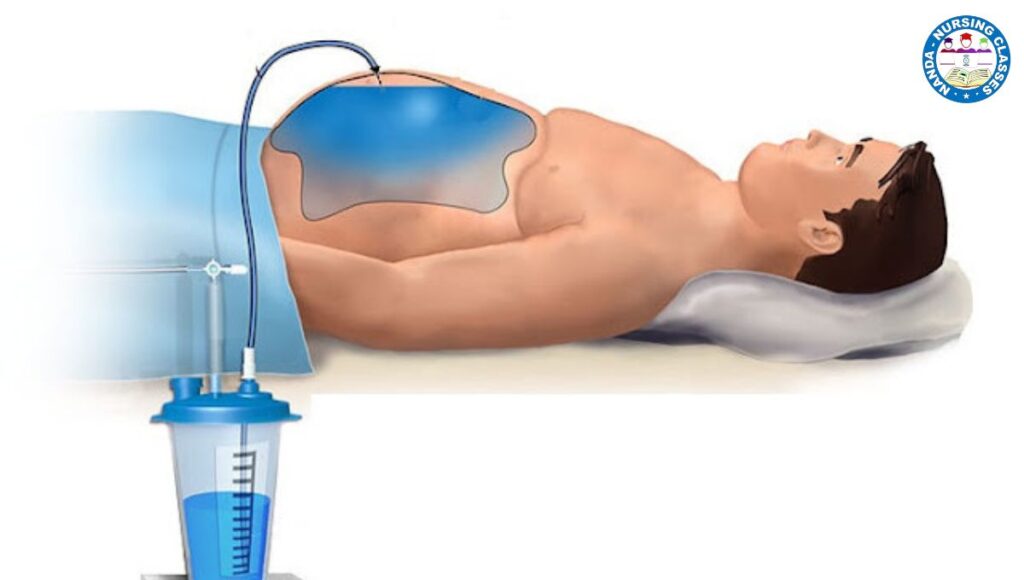
- Monitor vitals, pain control (PCA pump or opioids).
- Assess for bleeding (vaginal or incision site).
- Encourage early ambulation to prevent DVT.
- Foley catheter care (usually removed in 24-48 hrs).
Tracheostomy Care (If Airway Complication Occurs)
- Suction secretions as needed.
- Keep the stoma clean (sterile dressing changes).
- Monitor for infection or displacement.
Conclusion
A hysterectomy is a major surgical procedure requiring thorough nursing knowledge for optimal patient outcomes. Understanding indications, types, complications, preoperative and postoperative care ensures safe and effective patient management.
FAQs on Hysterectomy (USA-Based)
1. How long is recovery after a hysterectomy?
- Vaginal/Laparoscopic: 2-4 weeks
- Abdominal: 6-8 weeks
2. Will I go into menopause after a hysterectomy?
- Only if ovaries are removed (surgical menopause).
3. Can I have sex after a hysterectomy?
- Yes, after 6-8 weeks (once cleared by the doctor).
4. What are the alternatives to hysterectomy?
- Medications, myomectomy (fibroid removal), uterine artery embolization.
5. Does insurance cover a hysterectomy?
- Most US insurers cover medically necessary hysterectomies (check individual plans).
6. How much does a hysterectomy cost?
The cost of a hysterectomy varies widely depending on factors like surgical approach, location, insurance coverage, and medical complexity. Here’s a general breakdown:
Average Costs in the U.S. (2024 Estimates)
| Type of Hysterectomy | Cost Without Insurance | Cost With Insurance |
|---|---|---|
| Abdominal (Open) Hysterectomy | $15,000 – $25,000+ | $1,000 – $5,000 (copays/deductibles) |
| Laparoscopic Hysterectomy | $20,000 – $35,000+ | $1,500 – $6,000 |
| Robotic-Assisted Hysterectomy | $25,000 – $50,000+ | $2,000 – $7,000 |
| Vaginal Hysterectomy (Least invasive) | $10,000 – $20,000 | $800 – $4,000 |
What Influences Cost?
- Type of Surgery
- Open abdominal is usually cheaper (but longer recovery).
- Robotic/laparoscopic costs more due to advanced tech.
- Hospital vs. Outpatient Center
- Hospital stays add $3,000–$10,000/night.
- Outpatient (laparoscopic) can reduce costs.
- Insurance Coverage
- Medicare/Medicaid may cover most costs.
- Private insurance often covers 80–90% after deductible.
- Pre-authorization is usually required.
- Additional Fees
- Anesthesia ($1,000–$3,000)
- Pathology tests (if checking for cancer)
- Surgeon’s fees (varies by experience)
Ways to Reduce Costs
✔ Compare surgeons/hospitals (prices vary wildly).
✔ Ask about bundled pricing (some hospitals offer flat rates).
✔ Negotiate payment plans (hospitals often give discounts for upfront cash payments).
✔ Consider outpatient centers (if eligible for laparoscopic surgery).
International Cost Comparison
- Mexico/India/Thailand: $4,000–$10,000 (all-inclusive, but research quality).
- UK/Canada: Often free or low-cost under public healthcare (but long wait times).
Next Steps
- Call your insurance to verify coverage.
- Ask the surgeon’s office for a detailed estimate.
- Check if your hospital offers financial aid (nonprofits like Patient Advocate Foundation may help).
7. Advice for Husbands After Your Wife’s Hysterectomy
A hysterectomy is a major surgery, and your wife will need physical and emotional support during recovery. Here’s how you can help her heal—and strengthen your relationship through this transition.
1. Understand the Surgery & Recovery Timeline
- First 2 Weeks: She’ll need maximal rest (no lifting, driving, or chores).
- Weeks 3–6: Gradual improvement, but still no heavy activity or sex (doctor’s clearance needed).
- Full recovery may take 6–12 weeks (longer if abdominal surgery).
What to Do:
✔ Learn about her specific procedure (laparoscopic vs. abdominal).
✔ Track her pain meds and doctor’s instructions.
✔ Be patient—she may feel fatigued, emotional, or in discomfort for weeks.
2. Take Over Household Responsibilities
- Cook meals (focus on high-protein, high-fiber foods to aid healing).
- Handle chores (laundry, dishes, cleaning).
- Manage kids/pets (if applicable) so she can rest.
What NOT to Do:
✖ Don’t say “Let me know if you need help” (she may not ask). Instead, just do it.
✖ Don’t expect her to “push through” pain—rest is crucial.
3. Emotional Support Matters
- Hormonal shifts (if ovaries were removed) can cause mood swings, sadness, or anxiety.
- She may grieve loss of fertility (even if she didn’t want more kids).
- Body image concerns are common (scars, weight changes).
What to Say/Do:
✔ “I’m here for you—how are you feeling today?” (Listen without fixing.)
✔ Reassure her she’s still beautiful & loved.
✔ Encourage small joys (favorite shows, books, gentle walks).
What NOT to Say:
✖ “When can we have sex again?” (Wait for her doctor’s approval—usually 6+ weeks.)
✖ “At least you don’t have periods anymore!” (Minimizing her feelings isn’t helpful.)
4. Help with Physical Recovery
- Pain management: Keep track of meds, ice packs, heating pads.
- Mobility aid: Help her walk short distances (prevents blood clots).
- Incision care: Watch for signs of infection (redness, swelling, fever).
Red Flags to Report to the Doctor:
⚠ Heavy bleeding
⚠ Severe pain not relieved by meds
⚠ Fever or foul-smelling discharge
5. Navigate Intimacy Carefully
- No penetrative sex until cleared by her doctor (usually 6–8 weeks).
- Non-sexual affection (cuddling, holding hands) helps her feel connected.
- After clearance:
- Go slowly—she may have vaginal dryness (ask her doctor about lubricants or estrogen cream).
- Be mindful of emotional readiness (some women feel anxious about pain).
6. Plan for Long-Term Health
- If her ovaries were removed, she may need hormone replacement therapy (HRT).
- Encourage pelvic floor exercises (Kegels) once healed.
- Help her ease back into exercise (walking first, then gradual strength training).
Final Thought
Your support now will make a huge difference in her recovery. The more you step up without being asked, the smoother this journey will be.