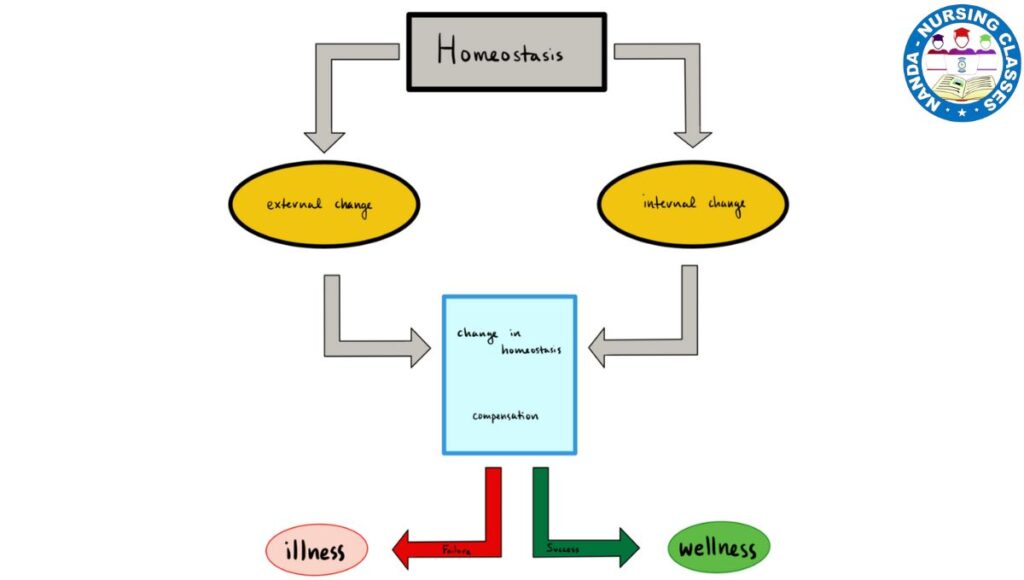
Homeostasis is a fundamental concept you must understand in nursing. It’s the body’s amazing, dynamic process of maintaining a stable and balanced internal environment, despite constant changes internally and externally. Think of it as the body’s own sophisticated control system, tirelessly working to keep everything in the perfect zone for health and function.
Table of Contents
Why is it called a “Balancing Act”?
Imagine these scenarios:
- 🥶🥵 Whether it’s freezing cold or scorching hot outside, your core body temperature stays remarkably constant at around 37°C (98.6°F).
- 🧃 You’ve just had a sugary drink, spiking your blood glucose, but within hours, your body brings it back to a normal range.
- 🏃♂️ You’ve just finished a run, and your heart is racing. Soon after you stop, your heart rate and breathing slow down to their resting rates.
All of this automatic regulation is thanks to homeostasis.
Why is Homeostasis So Important?
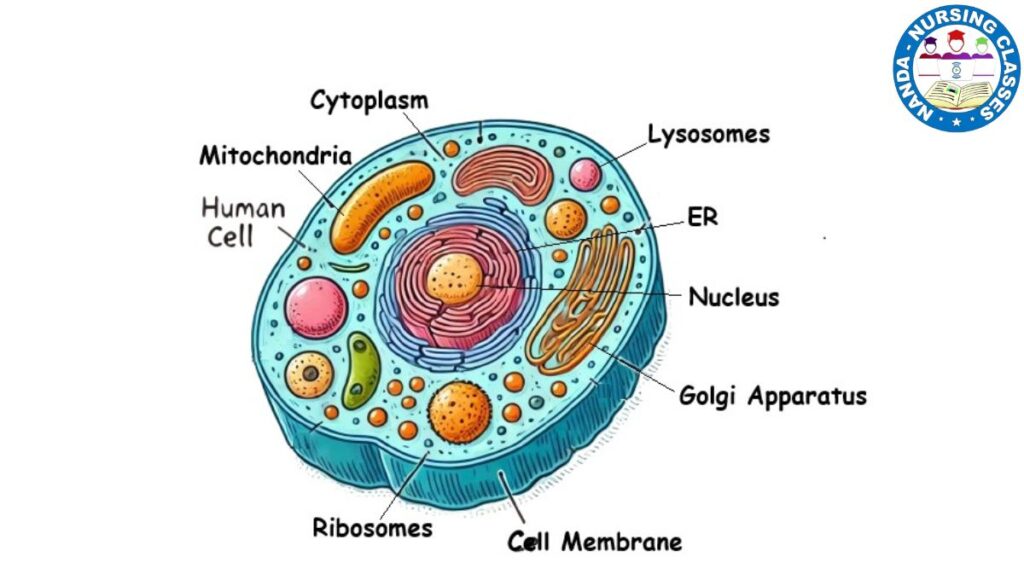
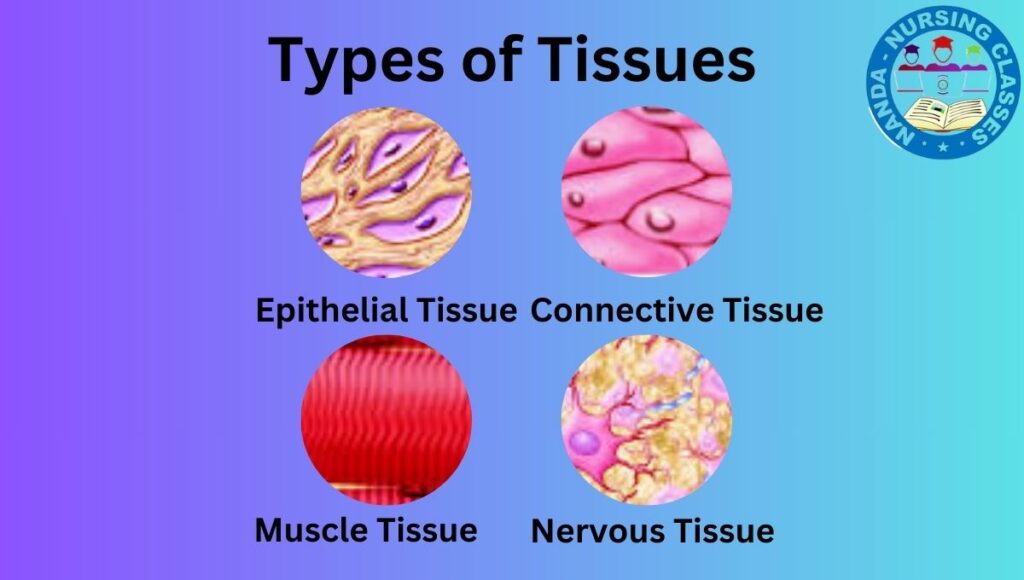
- Optimal Function: It provides the ideal environment for cells, tissues, and organs to perform their jobs efficiently.
- Protection: A stable internal environment helps the body withstand external stresses (like temperature changes) and internal challenges (like illness).
- Indicator of Health: When homeostasis is maintained, the body is healthy. When it is disrupted, disease or disorder follows. As a nurse, you will constantly care for patients whose bodies are struggling to maintain this balance.
The Control Mechanism: Feedback Loops
The body maintains homeostasis primarily through feedback loops. These are cycles where a change is detected, and a response is triggered to correct that change. Every loop involves specific components:
- Stimulus: The change that occurs.
- Receptor (Sensor): Monitors the environment and detects the change.
- Control Center: (Usually the brain) Receives information, interprets it, and determines the response.
- Effector: The organ or gland that carries out the response.
- Response: The action that alters the original stimulus.
There are two main types of feedback loops: Negative and Positive.
1. Negative Feedback Loop: The Standard
This is the most common mechanism in the body. Its goal is to reduce the effect of the original stimulus, effectively “negating” the change to return the system to its normal set point.
How it works: If a level gets too high, the body works to lower it. If it gets too low, the body works to raise it.
Simple Diagram:Stimulus (Change) → Receptor Detects → Control Center Processes → Effector Acts → Response (Returns to Normal)
Key Examples:
- Body Temperature Regulation (Thermoregulation):
- Stimulus: Body temperature rises above 37°C (e.g., from exercise, hot environment).
- Receptor: Thermoreceptors in the skin and brain detect the increase.
- Control Center: The hypothalamus in the brain.
- Effector: Blood vessels in the skin (dilate to release heat) and sweat glands.
- Response: Sweating increases; heat is lost through evaporation, cooling the body back to normal.
- Blood Glucose Regulation:
- Stimulus: Blood glucose rises after a meal.
- Receptor: Pancreas detects high glucose levels.
- Control Center: Pancreas.
- Effector: Pancreas releases insulin into the bloodstream.
- Response: Insulin signals cells to absorb glucose, lowering blood sugar back to the normal range.
2. Positive Feedback Loop: The Amplifier
This loop is less common and is used to amplify or intensify the original stimulus, pushing a process to completion. It does not maintain stability but creates a rapid change.
How it works: The response reinforces the initial stimulus, creating a self-amplifying cycle. It requires an external event to break the cycle.
Simple Diagram:Stimulus (Change) → Receptor Detects → Control Center Processes → Effector Acts → Response (Amplifies Stimulus) → Cycle Continues Until Broken
Key Examples:
- Childbirth (Labor and Delivery):
- Stimulus: Uterine contractions begin.
- Receptor: Pressure receptors in the cervix are stretched.
- Control Center: The pituitary gland in the brain.
- Effector: Pituitary gland releases more oxytocin.
- Response: Oxytocin causes stronger and more frequent contractions, which stretch the cervix further, leading to even more oxytocin release. This loop continues until the baby is born (the event that breaks the cycle).
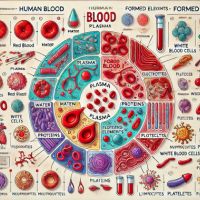
- Blood Clotting (Hemostasis):
- Stimulus: A blood vessel is damaged and bleeding occurs.
- Receptor: Platelets detect the injury and adhere to the site.
- Control Center: Damaged tissue and platelets release clotting factors.
- Effector/Response: The clotting factors attract more platelets and fibrin to form a clot. This process continues to amplify until a firm clot is formed and bleeding stops.
Nursing Correlation: Why This Matters to You
Understanding homeostasis is not just academic; it is the bedrock of clinical practice.
- Assessment: When you check vital signs (Temperature, Blood Pressure, Heart Rate, Respiratory Rate, Oxygen Saturation), you are directly assessing the state of a patient’s homeostasis. These are the key indicators the body works hardest to control.
- Diagnosis: A fever (hyperthermia), low blood pressure (hypotension), or high blood sugar (hyperglycemia) are all clear signs that homeostasis has been disrupted. Your job is to figure out why.
- Intervention: Your nursing actions are often designed to support the body’s homeostatic mechanisms. This includes:
- Administering antipyretics (e.g., Tylenol) to help lower a fever.
- Providing IV fluids to help raise blood pressure.
- Giving insulin to a diabetic patient to help regulate blood sugar.
- Patient Education: You teach patients with chronic illnesses (like diabetes or hypertension) how their lifestyle and medications help their body maintain balance, empowering them to manage their own health.
In summary, homeostasis is the silent, continuous process that defines health. As a nurse, you are the key observer and supporter of this incredible balancing act.
FAQs on Homeostasis: The Body’s Balancing Act
1. What is homeostasis in simple terms?
Homeostasis is the body’s ability to maintain a stable and constant internal environment, even when outside conditions change. Think of it like the thermostat in your house. If the temperature drops, the heater turns on; if it gets too hot, the AC kicks in. Your body constantly makes similar tiny adjustments to keep things like temperature, blood sugar, and water levels perfectly balanced.
2. Why is homeostasis important?
It is essential for survival. Our cells need a very specific environment to function correctly. If conditions like temperature or pH shift too much, enzymes stop working, cells can’t communicate, and organs fail. Homeostasis provides that optimal, stable environment, protecting us from disease and allowing our bodies to cope with stress and change.
3. What are some examples of homeostasis in the body?
- Body Temperature: Maintaining ~37°C (98.6°F) by sweating when hot and shivering when cold.
- Blood Glucose: Regulating blood sugar levels through the hormones insulin (which lowers sugar) and glucagon (which raises it).
- Water Balance (Osmoregulation): Controlling water levels through thirst and kidney function, adjusting urine concentration.
- Blood Pressure: Adjusting heart rate and narrowing/widening blood vessels to maintain stable pressure.
- Calcium Levels: Using hormones to pull calcium from bones or store it to keep blood calcium levels stable.
4. What’s the difference between negative and positive feedback loops?
This is a key distinction:
- Negative Feedback Loops are like a thermostat. They reverse a change to bring the body back to its “set point.” This is the most common type, used for temperature, blood sugar, and blood pressure control. (e.g., High blood sugar → Insulin released → Blood sugar lowers).
- Positive Feedback Loops are like a snowball effect. They amplify a change to complete a specific process. These are less common and are not used for day-to-day balance. (e.g., Labor contractions → Oxytocin released → Stronger contractions → Baby delivered).
5. Is a fever a failure of homeostasis?
Not exactly. A fever is actually a controlled reset of the body’s thermostat in the brain (hypothalamus) to help fight infection. It’s a deliberate, temporary change in the “set point.” So, the body is still maintaining homeostasis, just at a higher temperature to create a less favorable environment for pathogens. It becomes a problem only if the temperature gets dangerously high.
6. How do diseases relate to homeostasis?
Most diseases are a disruption of homeostasis. The body can no longer maintain balance on its own.
- Diabetes: The negative feedback loop for blood sugar is broken. The pancreas doesn’t produce enough insulin, or the body doesn’t respond to it, leading to chronically high blood glucose.
- Hypertension (High Blood Pressure): The mechanisms that regulate blood pressure (like vessel constriction/dilation) are malfunctioning, forcing the heart to work harder.
- Dehydration: The body loses more water and electrolytes than it takes in, disrupting the balance of fluids and minerals needed for cellular function.
7. How does understanding homeostasis help nurses?
It is the foundation of all nursing care. Nurses:
- Assess: Vital signs (TPR, BP, O2 sat) are direct measurements of homeostatic processes.
- Diagnose: Recognizing that abnormal vitals or lab values (e.g., high glucose, low sodium) mean homeostasis is disrupted.
- Intervene: Nursing actions (giving fluids, administering insulin, providing antipyretics) are designed to support the body’s efforts to regain balance.
- Educate: Teaching patients with chronic illnesses how their treatments (diet, medication) help restore and maintain their body’s balance.
8. Can we consciously control homeostasis?
For the most part, no. Homeostatic processes are involuntary and controlled by the autonomic nervous system and endocrine system. You don’t consciously tell your pancreas to release insulin. However, some behaviors that support homeostasis are conscious, such as drinking water when you feel thirsty, putting on a jacket when you’re cold, or eating a snack if your blood sugar is low.
9. What organ is most responsible for homeostasis?
While it’s a whole-body effort, the brain is the master coordinator. Specifically, a region called the hypothalamus acts as a central control center. It receives information from sensors throughout the body and coordinates responses via the nervous and endocrine systems to regulate temperature, hunger, thirst, sleep, and fluid balance.
10. Is homeostasis the same as equilibrium?
No. Equilibrium implies a passive, static balance where everything is equal. Homeostasis is a dynamic, active process that requires energy. It’s not about being “equal” to the outside environment but about maintaining a difference—a special internal state that is different from and more stable than the outside world. The body is constantly reacting and adjusting to maintain this state.