Introduction
The amputation bed procedure is a critical component of nursing care for patients who have undergone limb amputation. Nursing students must grasp the intricacies of this procedure to provide effective post-operative care that promotes healing, minimizes complications, and supports patients’ physical and emotional recovery.
Amputation – The method of cutting any limb by surgical method.
Table of Contents
Definition of Amputation Bed
The amputation bed procedure encompasses a series ofsteps aimed at ensuring the proper positioning, wound care, and psychological support for patients who have undergone limb amputation. This procedure facilitates optimal healing and overall well-being.
Amputation Bed-Making Purposes
The key objectives of the amputation bed procedure are:
Patient Comfort: Positioning patients to alleviate pain and discomfort.
Wound Healing: Creating an environment conducive to wound healing and preventing infection.
Contracture Prevention: Preventing joint contractures in the residual limb.
Edema Management: Minimizing edema through elevation and appropriate positioning.
Psychosocial Support: Providing emotional support to enhance patient coping and recovery.
Principles of Amputation Bed Making
Creating an appropriate amputation bed is a fundamental aspect of patient care after limb amputation. Following the principles outlined below ensures the patient’s comfort, promotes healing, and minimizes the risk of complications.
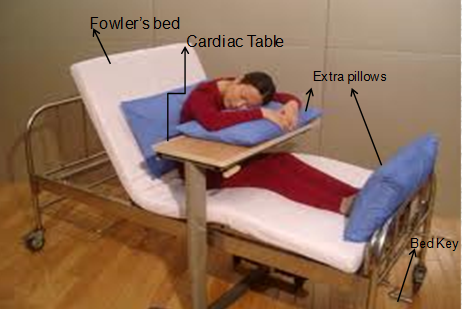
- Proper Positioning:
Position the patient’s residual limb (the amputated limb) to maintain alignment with the body while avoiding pressure on the wound site. Use pillows strategically to support the limb and alleviate pressure on vulnerable areas.
- Elevation:
Elevate the foot of the bed using an elevated footrest or similar device. This elevation helps reduce edema (swelling) in the residual limb and enhances blood circulation, which is crucial for wound healing.
- Bed Cradle Use:
Place a bed cradle over the residual limb. The bed cradle keeps bedding from coming into direct contact with the limb, minimizing the risk of pressure ulcers and protecting the wound site.
- Pain Management:
Administer prescribed pain medications as directed. Adequate pain management is vital for patient comfort and facilitates mobility and participation in rehabilitation activities.
- Wound Care Compliance:
Follow the surgeon’s instructions for wound care, including dressing changes, antiseptic application, and monitoring for signs of infection. Adhering to the wound care regimen promotes optimal healing.
- Range of Motion Exercises:
Encourage and assist the patient with gentle range of motion exercises on the non-amputated limb. These exercises prevent joint contractures and maintain flexibility during the recovery process.
- Psychological Support:
Offer emotional support and reassurance to the patient. Address any concerns they may have about their recovery, body image, or future mobility.
- Patient Education:
Educate the patient about the importance of proper positioning, wound care, and early mobility. Empower them to actively participate in their care and take ownership of their recovery journey.
- Monitoring and Assessment:
Regularly assess the patient’s wound healing progress, pain levels, and overall well-being. Monitor for any signs of infection, poor circulation, or other complications.
- Collaborative Care:
Work closely with the interdisciplinary healthcare team, including surgeons, physical therapists, and psychologists, to ensure comprehensive and coordinated care for the patient.
- Individualization:
Tailor the amputation bed setup and care plan to each patient’s specific needs and condition. No two patients are exactly alike, and personalized care enhances outcomes.
- Communication:
Maintain open and transparent communication with the patient, their family members, and the healthcare team. This promotes a collaborative and supportive care environment.
Incorporating these principles into amputation bedmaking contributes to the patient’s well-being, supports their recovery, and enhances their quality of life as they adapt to their new circumstances.
Equipment required for Amputation Bed Making
Essential equipment for the amputation bed procedure includes:
Pillows: Supporting proper limb positioning and pressure relief.
Bed Cradles: Preventing bedding from contacting the residual limb.
Elevated Footrest: Elevating the residual limb to reduce edema.
Analgesics: Administering prescribed pain medications.
Wound Care Supplies: Dressings, antiseptics, and bandages for wound care.
Amputation Bed-Making Procedure
The Procedure of an Amputation bed is described below but when we are making an amputation bed for the patient we have to make a normal bed first.
| Steps of procedure | Rationale |
|---|---|
| 1. Prepare the bed for a simple bed until the draw sheet is in position. | Because the bed is required. |
| 2. The top sheet is placed over the patient’s chest, and trunk. |
To maintain privacy and to provide warmth to the patient. |
| 3. The narrow mackintosh and narrow sheet are placed over the thing and held firmly placing the sandbags over it at either side of the thigh. | To protect the linen and sandbag, to immobilize the painful joints. |
| 4. The cradle is then placed over the stump. | To keep the weight of the bedclothes from pressing |
| 5. The two parts may be folded slightly back | To visualize the stump without disturbing the bed |
| 6. The two sections of the top linen should overlap each other at least by 8 to 10 inches. | To observe the stump and also to prevent unnecessary exposure of the patient. |
To follow these process steps you will make an amputation bed and the below points kept in mind
- Patient Assessment:
Evaluate the patient’s condition, surgical history, and residual limb condition.
- Positioning:
Place pillows strategically for residual limb support while avoiding pressure on the wound.
- Bed Cradle:
Install a bed cradle to keep bedding from touching the residual limb.
- Pain Management:
Administer prescribed pain medications and monitor effectiveness.
- Wound Care:
Adhere to surgeon’s instructions for wound dressing changes and antiseptic application.
- Range of Motion Exercises:
Perform gentle exercises on the non-amputated limb to prevent contractures.
- Patient Education:
Instruct patients on proper positioning, wound care, and early mobility benefits.
- Psychosocial Support:
Offer emotional support and address psychological concerns.
After Care Articles
After the care of a patient or after making of amputation bed you have to replace, discard, or properly set up all articles that you used in the procedure.
Nursing Considerations
Assessment: Regularly assess wound healing progress, pain levels, and psychological state.
Mobility: Encourage early mobility and assistive device adaptation when necessary.
Emotional Care: Listen actively, provide reassurance, and offer counseling support.
Complication Vigilance: Monitor for signs of infection, impaired circulation, or complications.
Education: Ensure patients comprehend care plans and self-care routines.
Conclusion
The amputation bed procedure is a pivotal element of nursing care, combining positioning, wound management, and emotional support for amputee patients. Nursing students’ adept execution of this procedure contributes significantly to patients’ successful recovery.
Exam Question
- Explain the rationale behind the amputation bed procedure’s key objectives and outline the procedural steps to provide comprehensive care for a patient after limb amputation.
- How does the amputation bed procedure contribute to preventing joint contractures?
- What are the essential components of patient education following limb amputation, and why is it crucial?
FAQs (Frequently Asked Questions)
- Why is using a bed cradle important in the amputation bed procedure?
A bed cradle prevents bedding from making direct contact with the residual limb, reducing the risk of pressure ulcers and promoting optimal healing conditions.
- How can nursing students help manage phantom limb pain in amputee patients?
Nursing students can collaborate with the healthcare team to administer pain medications, implement relaxation techniques, and provide psychological support to alleviate phantom limb pain.
- What role does patient education play in the amputation bed procedure?
Patient education empowers patients to actively participate in their care, understand wound care routines, and make informed decisions about their recovery journey.
- How frequently should wound dressings be changed in the amputation bed procedure?
The frequency of dressing changes depends on the surgeon’s recommendations and the wound’s condition. Regular assessments help determine the appropriate interval for dressing changes.
Remember, mastering the amputation bed procedure demands a comprehensive understanding of wound care, psychological support, and patient-centered care principles.