Paracentesis is a clinical procedure in which a needle is inserted into the peritoneal cavity of the patient and his or her ascetic fluid is removed from the peritoneal cavity by a skilled healthcare worker. Paracentesis is a medical procedure used to remove fluid from the body. It is typically done to help diagnose or treat a medical condition. The most common type of paracentesis is abdominal paracentesis, which is used to remove fluid from the abdomen. This can help diagnose and treat conditions such as ascites (excess fluid in the abdomen due to liver disease) and abdominal infections. Other types of paracentesis include thoracic and joint paracentesis, which are used to remove fluid from the chest or joints, respectively. Paracentesis can also be used to remove excess fluid from the eye or to help diagnose or treat a heart condition.
Now it’s time to know what is the reason for the accumulation of fluid in a person’s abdomen cavity and why there is a need for Paracentesis?
The most common cause of accumulation of fluid is liver cirrhosis of the person. Drinking too much alcohol is one of the most common causes of liver cirrhosis in the person. This condition is known as ascites.
Different types of cancer can also cause this condition. Ascites caused by cancer most often occur with advanced or recurrent cancer. Ascites may also be caused by other problems such as heart conditions, dialysis, low protein levels, and infection.
In this condition of a person, there is a need for Paracentesis for diagnostic purposes in that we check the type of infection and, for therapeutic purposes, we check certain types of cancer, and to relieve the pressure of the abdomen and Improve kidney, bowel or respiratory function of the patient.
Definition of Paracentesis
Here are some definitions of Paracentesis are as follows:
“A surgical puncture of a bodily cavity (as of the abdomen) with a trocar, aspirator or other instruments usually to draw off an abnormal effusion for diagnostic or therapeutic purposes.”
(Dorland’s pocket medical dictionary)
“Abdominal Paracentesis is the removal of fluid from the peritoneal cavity through a small puncture made through the abdominal wall under sterile condition.”
(Annamma Jacob)
“Abdominal Paracentesis is the surgical removal of the abdominal fluid and relieve symptoms.”
(Lippincott)
“Abdominal Paracentesis means removal of fluid from the peritoneal cavity in cases of ascites due to hepatitis, cirrhosis of the liver, or in cases of peritonitis”
(Nanda-Nursing)
Purpose of Paracentesis
To make a diagnosis:- To study the chemical, bacterial and cellular composition of the peritoneal for the diagnosis. What Are the Possible Diagnostic Results of an Abdominal Tap? The most common cause of abdominal fluid requiring a diagnostic abdominal tap is cirrhosis of the liver. Other possible results and causes of fluid retention are:
- Infection
- Kidney disease
- Bowel damage
- Heart disease
- Pancreatic disease
- Tumour
- To relieve pressure on the abdominal and chest organs when a transuded collected as a result of renal, cardiac, or liver disease.
To drain:- An exudate is drained in ascites and peritonitis.
To give treatment:- In case of pulmonary tuberculosis affecting the base of the lungs, fluid is removed and the air is instilled to create artificial pneumothorax.
Indications of abdominal Paracentesis
There are several generally accepted indications for abdominal Paracentesis:
- Evaluation of new-onset ascites
- Testing of ascetic fluid in a patient with preexisting ascites who is admitted to the hospital, regardless of the reason for admission
- Evaluation of a patient with ascites who has signs of clinical deterioration, such as fever, abdominal pain/tenderness, hepatic encephalopathy, peripheral leukocytosis, deterioration in renal function, or metabolic acidosis
Contraindications of abdominal Paracentesis
However, there are some relative contraindications to abdominal Paracentesis:
- Patients with clinically apparent disseminated intravascular coagulation and oozing from needle sticks. This occurs in <1/1000 patients with ascites in our experience.
- Primary fibrinolysis (which should be suspected in patients with large, three-dimensional bruises). Paracentesis can be performed once the bleeding risk is reduced with treatment.
- Paracentesis should not be performed in patients with massive ileum with bowel distension unless the procedure is image-guided to ensure that the bowel is not entered.
How much fluid aspirate in Paracentesis?
The amount of Paracentesis is depend on the purpose of the Paracentesis of the patient, here are some measurements of the amount of fluid to aspirate by Paracentesis are as described:
- Diagnostic Paracentesis refers to the removal of a small quantity of fluid for testing.
- Therapeutic Paracentesis refers to the removal of 5 litres or more of fluid to reduce intra-abdominal pressure and relieve the associated dyspnea, abdominal pain, and early satiety.
Articles used in Paracentesis
A cover sterile tray containing:-
- Sterile gloves
- sponge holding forceps
- 5c.c. holding forceps
- 20 c.c. a syringe with needles for local anaesthesia
- 3-way adopter and tubing
- tracer and canola or aspiration needles
- small bowel for cleaning lotion
- specimen collection bottles
- sterile dressing towel
- dressing material –cotton swabs, pieces and coo ten pad
- gloves gown, and mask
Occasionally an incision is made for Paracentesis:-
The following articles are required for that
- B.P. handle with blade
- suture and skin needles
- Suture scissors.
- Artery forceps
- Needle holder
An unsterile tray containing articles for Paracentesis
- Macintosh and draw sheet
- Spirit, Iodine or chlorhexidine,
TR. Benzoic - Bucket to collect the fluid
- Kidney tray and paper bag
- Pint measure
- Abdominal binder and pins
- A glass with stimulates mixture.
- Backrest and pillow.
Choice of Paracentesis needle
The choice of the needle depends upon whether a diagnostic or therapeutic paracentesis is planned. As a general rule, the narrowest needle should be used to minimize complications in the event that a blood vessel or the bowel is entered by the needle. A diagnostic paracentesis can be performed in a lean patient with a 1 or 1.5 inches 22-gauge needle, while a 3.5-inch 22-gauge “spinal” needle can be used for diagnostic paracentesis in an obese patient. For a
therapeutic paracentesis, a larger, 15- or 16-gauge needled is used to speed the removal of ascetic fluid.
General instruction for Paracentesis
- Explain the procedure thoroughly to the patient and his relatives to get the co-operation. Co- operation is necessary to prevent injury to the adjacent organs.
- Obtain written consent from the patient and relatives
- Ask the patient to urinate 5 minutes before the procedure to avoid injury to the urinary bladder
- Shave the abdominal to clean the skin. Use antiseptic to cleanse the abdominal area.
- Follow strict aseptic techniques to prevent the introduction of infection into the peritoneal cavity.
- Keep the emergency injection tray ready to prevent vascular shock. To prevent the shock.
- Withdraw the fluid slowly
- Withdraw a small quantity of fluid at a time
- Apply pressure on the abdomen with an abdominal binder and tighter it from above downward as the fluid is drained.
- Keep the patient warm. Observe the vital sign throughout the procedure.
- Control the flow of fluid by using clamps on the tubing
- Seal the wound immediately after the procedure to prevent infection and leakage of peritoneal fluid.
Patient preparation for Paracentesis
- Signed consent form.
- Patient preparation consists of explaining the procedure to the patient and obtaining informed consent. Patients do not need to be fasting before the procedure. We have performed thousands of paracenteses and have never held food or fluids by mouth in advance of the procedure.
Paracentesis procedure
PREPARATORY PHASE
- Explained the procedure to the patients.
- Record the patient’s vital signs
- Have the patient void before treatment is begun. Make sure that the consent form has been signed.
- Position the patient in fowler‘s position with his back arms and feet supported
- Drop the patient with a sheet exposing the abdomen.
PERFORMANCE PHASE
- Assets in preparing skin with an antiseptic solution.
- Open sterile tray and package of sterile gloves provide the athletic solution
- Have collection bottles and tubing available
- Assess pulse and respiratory status frequency during the procedure and watch for pallor, cyanosis, or syncope.
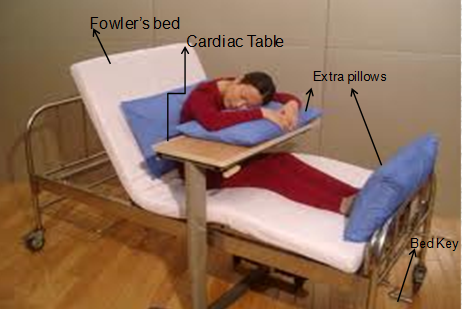
- The physician administers local anaesthesia and introduces needles or trocar.
- A needle or trocar is connected to tubing and a vacuum bottle or syringe, and fluid is slowly drained from the peritoneal cavity.
- Apply to dress when the needle is withdrawn.
FOLLOW-UP PHASE
- Assist the patient to a comfortable position after treatment
- Record the amount and characteristics of fluid removed, the number of specimens sent to the laboratory, and the patient’s condition during treatment.
- Check blood pressure and vital signs every ½ hours for 2 hours, every hour for 4 hours, and every 4 hours for 24 hours.
- Usually, a dressing is sufficient; however, if the trocar wound appears large, the physician may close the incision with sutures.
- Watch for leakage or scrotal oedema after Paracentesis.
After care of the Paracentesis patient
- When pressure symptoms are relieved/enough fluids is withdrawn the canola is removed.
- Seal the puncture wound with tr. Benzoic cover with pad to prevent leakage.
- Tighten the abdominal bandage to maintain abdominal pressure.
- Send the specimen to the laboratory with a labelled and requisition form
- Watch the patient for reaction during the day.
- Clean them with soap and water, dry and send them for autoclaving.
Complications of Paracentesis
- Ascetic fluid leak
- Bleeding
- Bowel perforation and infection
- Mortality
Conclusion
Rapid diagnosis and treatment play a key role in the management of Spontaneous Bacterial Peritonitis. In general, potentially fatal cirrhosis-related infectious disease is diagnosed based only on an increased PMN count in the ascitic fluid, and the identification of the causal pathogen is sometimes not taken into consideration. Although no ideal method for detecting causal bacteria has been established, our novel ISH test may be used to provide early and direct
evidence of bacterial infection in Spontaneous Bacterial Peritonitis patients with ascites. The current findings, therefore, shed new light on the management of Spontaneous Bacterial Peritonitis.
Paracentesis is a medical procedure used to remove fluid from the abdominal cavity. The fluid can be used to diagnose and treat a variety of medical conditions. It is most commonly used to diagnose and treat ascites, a condition in which fluid accumulates in the abdomen. It is also used to treat infections, cancer, and bleeding.
The procedure involves inserting a needle into the abdominal cavity to draw out fluid. Before the procedure, the patient is given a local anesthetic to numb the area. During the procedure, a thin needle is inserted into the abdominal wall and the fluid is slowly suctioned out. The amount of fluid removed depends on the condition being treated and the amount of fluid present in the abdomen.
Following the procedure, the patient may experience some discomfort and may need to take a break from activities that involve vigorous movement. Recovery time depends on the amount of fluid removed and the underlying condition. In most cases, individuals can return to their normal activities within a few days.
Paracentesis is a safe and effective procedure, but it should be performed by a qualified medical professional. The risks of the procedure include infection, bleeding, and damage to surrounding organs. To reduce the risk of complications, it is important to follow the doctor’s instructions carefully.
FAQs
What is a paracentesis?
Paracentesis is a medical procedure used to remove fluid buildup in the abdominal cavity (ascites) by inserting a needle or catheter into the abdomen.
Why is a paracentesis performed?
Paracentesis is typically performed to relieve symptoms associated with ascites, such as abdominal pain, difficulty breathing, and swelling.
How is a paracentesis performed?
During the procedure, the patient typically lies on their back while a healthcare provider cleans and numbs the abdomen. A needle or catheter is then inserted into the abdominal cavity to drain the excess fluid.
Is a paracentesis painful?
The procedure is usually well-tolerated, as local anesthesia is used to numb the area. Some patients may experience mild discomfort or pressure during the insertion of the needle.
Are there any risks associated with paracentesis?
While paracentesis is generally safe, there are some risks, including bleeding, infection, and injury to nearby organs. However, these complications are rare.
How long does a paracentesis take?
The procedure typically takes about 30 minutes to an hour to complete, including preparation and recovery time.
What happens after a paracentesis?
After the procedure, the patient may be monitored for a short time to ensure there are no complications. They may also be advised to rest and avoid strenuous activity for the remainder of the day.
How much fluid can be removed during a paracentesis?
The amount of fluid removed depends on the individual patient’s condition and the physician’s recommendation. Typically, between 4 to 6 liters of fluid can be safely removed during one procedure.
Is paracentesis always necessary for ascites?
Paracentesis may not be necessary for all cases of ascites. It is usually recommended when the fluid buildup is causing significant symptoms or complications.
Can paracentesis be repeated?
Yes, paracentesis can be repeated as needed to manage ascites and relieve symptoms. The frequency of the procedure will depend on the patient’s condition and response to treatment.
If you have any queries Feel free to ask any Queries in the comment section 👇and share them with your PEAR groups
Share with your friends because “ Knowledge grows by sharing ”