A tracheostomy is a life-changing medical procedure that can feel overwhelming for patients and their loved ones. Whether you’re facing this procedure due to a planned medical treatment or emergency circumstances, understanding what to expect can help reduce anxiety and improve outcomes. This comprehensive guide will walk you through everything you need to know about tracheostomies, from the initial procedure to long-term care and quality of life considerations.
Introduction: Understanding Tracheostomy
What is a tracheostomy?
A tracheostomy is a surgical procedure that creates an opening (called a stoma) in the front of the neck, directly into the trachea (windpipe). A tracheostomy tube is then inserted through this opening to provide an alternative airway for breathing. This procedure bypasses the mouth and nose, allowing air to enter directly into the lungs.
Tracheostomies are performed for various medical reasons, including prolonged mechanical ventilation, severe breathing difficulties, airway obstruction, or when patients cannot protect their airways naturally. According to current medical guidelines, the Eastern Association of Surgical Trauma (EAST) recommends early tracheostomy (3-7 days after intubation) for patients with severe closed-head injuries and those requiring long-term ventilator support.
The Procedure: What to Expect
Emergency vs. Elective Tracheostomy
The approach to tracheostomy varies significantly depending on whether it’s performed as an emergency or elective procedure:
Emergency Tracheostomy is performed when there’s a sudden, life-threatening airway problem. These situations require immediate intervention and may occur in emergency rooms or intensive care units. The procedure must be completed quickly to restore breathing, and there’s often little time for extensive preparation or family consultation.
Elective Tracheostomy is a planned procedure, typically recommended when healthcare providers anticipate the need for long-term ventilator support or when chronic health conditions affect breathing. This allows for proper preparation, family education, and detailed discussion of the procedure and expected outcomes.
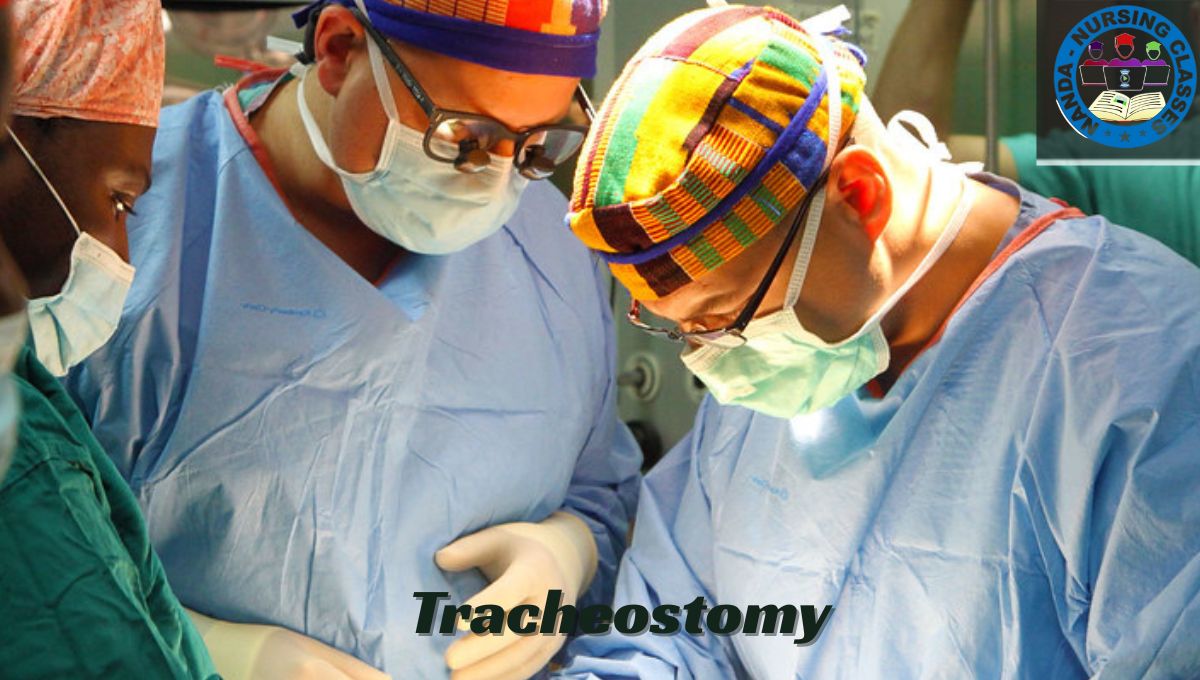
The Surgical Process
During the procedure, which is typically performed under general anesthesia, the surgeon makes a horizontal incision in the lower neck. The procedure involves careful dissection of neck tissues and creating an opening between the second and third tracheal rings. A tracheostomy tube is then inserted and secured in place.
The entire procedure usually takes 20-45 minutes, depending on the complexity of the case and the patient’s anatomy. Modern techniques have made the procedure safer and more standardized, with complications occurring in 40-50% of cases, but life-threatening complications in only about 1% of cases.
Post-Operative Care: Hospital to Home Transition
Immediate Hospital Care
The first few days after a tracheostomy are critical for healing and learning new care routines. In the hospital, your medical team will:
- Monitor the surgical site for proper healing
- Ensure the tracheostomy tube is functioning correctly
- Begin teaching basic care techniques
- Manage pain and any immediate complications
- Coordinate with speech therapists for communication strategies
Patients typically experience neck soreness and may have trouble swallowing for the first few days. It usually takes 2-3 days to adjust to breathing through the tracheostomy tube rather than through the nose and mouth.
Preparing for Home Care
Before discharge, patients and caregivers must demonstrate competency in essential care skills. This includes:
- Tracheostomy cleaning and maintenance: Learning to clean around the stoma site and change dressings
- Inner cannula care: Understanding how to remove, clean, and replace the inner tube
- Suctioning techniques: Mastering the use of suction equipment to clear secretions
- Emergency procedures: Knowing what to do if the tube becomes blocked or dislodged
Healthcare teams typically provide comprehensive training and practice sessions to ensure families feel confident with these skills before the patient goes home.
Living with a Tracheostomy: Daily Life Adaptations
Communication and Speaking
One of the most significant adjustments for tracheostomy patients involves communication. Initially, many patients cannot speak because air bypasses the vocal cords. However, several solutions can restore the ability to communicate:
Speaking Valves: The Passy-Muir valve is a one-way speaking valve that redirects airflow through the vocal folds, mouth, and nose, allowing for speech production. These valves have revolutionized communication for tracheostomy patients and can significantly improve quality of life.
Alternative Communication Methods: When speaking valves aren’t suitable, patients may use:
- Writing boards or tablets
- Communication apps on smartphones or tablets
- Sign language or gestures
- Computer-based communication devices
Eating and Dietary Considerations
Eating with a tracheostomy requires special considerations due to changes in swallowing mechanics. The presence of a tracheostomy tube can affect the normal swallowing process, potentially leading to increased risk of aspiration.
Key dietary considerations include:
- Swallowing Assessment: Speech-language pathologists typically evaluate swallowing safety before allowing oral feeding
- Texture Modifications: Many patients initially require modified textures (pureed foods, thickened liquids) to reduce aspiration risk
- Supervised Eating: Caregivers should always observe patients while eating to ensure food doesn’t enter the trach
- Gradual Progression: Most patients can eventually return to normal diets as they adapt and heal
Research shows that early involvement by speech-language pathologists leads to faster return to oral intake and improved tolerance of oral diets, improving patient outcomes and quality of life.
Activities of Daily Living
Living with a tracheostomy requires adaptations but doesn’t necessarily limit most activities:
Bathing and Showering: Special precautions prevent water from entering the tracheostomy. Shower shields and careful positioning help maintain hygiene while keeping the stoma dry.
Exercise and Physical Activity: Patients should avoid strenuous activity for 6 weeks after surgery, but most can gradually return to normal physical activities with proper precautions.
Work and Social Activities: Many patients successfully return to work and maintain active social lives. The key is learning to manage the tracheostomy confidently and having appropriate supplies available.
Potential Complications and Emergency Management
Common Complications
Understanding potential complications helps patients and caregivers respond appropriately:
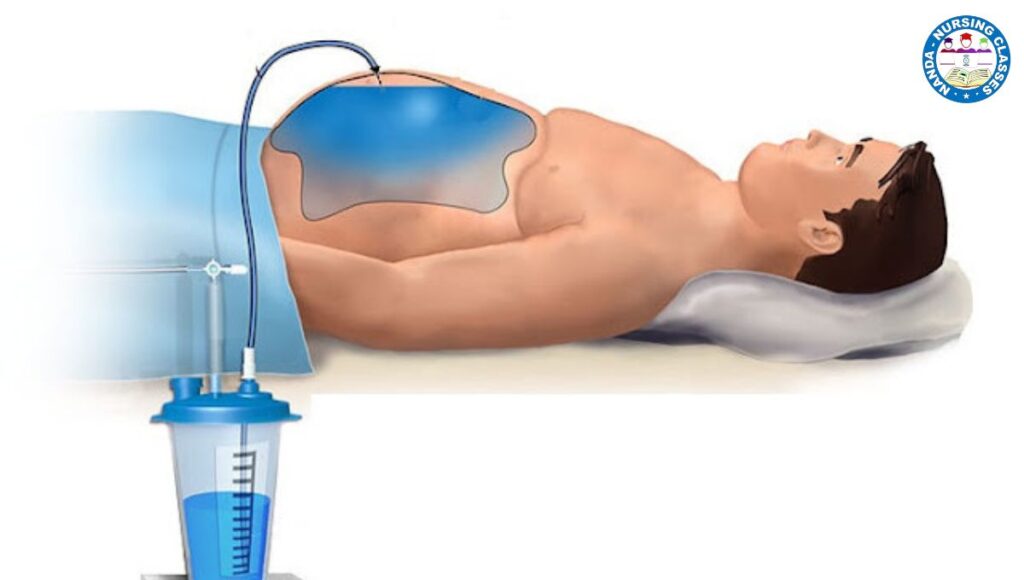
Tube Obstruction: The most common complications include obstruction of the tracheostomy (19%), which requires immediate attention. Signs include difficulty breathing, increased work of breathing, and inability to suction.
Infection: Infection occurs in approximately 14% of cases and may present as redness, swelling, increased drainage, or fever around the stoma site.
Bleeding: Bleeding complications occur in about 16% of patients and can range from minor bleeding around the stoma to more serious hemorrhage.
Accidental Decannulation: Tube dislodgement happens in approximately 13% of cases and constitutes a medical emergency requiring immediate intervention.
Emergency Management
Patients and caregivers should be prepared for emergency situations:
- Immediate Actions: Sit the patient upright, administer high-flow oxygen if available, and seek emergency medical attention
- Emergency Supplies: Keep emergency supplies readily available, including spare tracheostomy tubes, suction equipment, and emergency contact information
- Communication with EMS: Inform emergency responders about the tracheostomy immediately, as this affects their assessment and treatment approach
Tracheostomy Cost and Financial Considerations
Understanding Tracheostomy Costs
The financial impact of tracheostomy care can be significant, but understanding insurance coverage and available resources helps families plan effectively:
Initial Procedure Costs: For patients without health insurance, a tracheostomy and associated hospital stay typically costs $10,000-$150,000 or more, depending on the complexity and length of stay. Recent data shows the average cost for tracheostomy procedures is approximately $60,000.
Ongoing Supply Costs: Monthly supplies for tracheostomy care can be expensive, but most insurance plans provide coverage for essential supplies.
Insurance Coverage and Medicare Benefits
Medicare Coverage: Tracheostomy supplies are covered under the Prosthetic Benefit, with specific guidelines for covered quantities and replacement schedules. A tracheostomy care starter kit (A4625) is covered following surgical tracheostomy, with ongoing supplies covered beginning two weeks post-operatively.
Private Insurance: Research shows that 98.1% of studied insurance plans across 11 major insurers offer tracheostomy-related durable medical equipment coverage in some form, though co-pays and deductibles may apply.
Recent Trends: Medicare reimbursement for tracheostomy procedures has decreased, with a 20.3% inflation-adjusted decrease in reimbursement per planned tracheostomy, which may affect provider availability and patient access to care.
Financial Assistance Resources
Several resources can help families manage tracheostomy-related expenses:
- Hospital Financial Counselors: Most hospitals have financial counselors who can help navigate insurance coverage and identify assistance programs
- Manufacturer Programs: Companies that produce tracheostomy supplies often offer patient assistance programs
- Non-Profit Organizations: Various organizations provide grants and support for medical equipment and supplies
- State Medicaid Programs: Many states have expanded Medicaid coverage that includes durable medical equipment
Cost Planning
When planning for tracheostomy care costs, consider these high-value aspects:
- Tracheostomy supplies Medicare coverage: Understanding monthly allowances and replacement schedules
- Durable medical equipment insurance: Navigating coverage for suction machines, humidifiers, and other equipment
- Home healthcare services: Costs for professional nursing care and respiratory therapy services
- Emergency preparedness: Budgeting for backup equipment and emergency supplies
Quality of Life and Long-Term Outcomes
Adapting to Life Changes
Research on quality of life after tracheostomy reveals important considerations. Studies show that the most prominent changes patients experience include decreased sense of smell, decreased taste, decreased enjoyment of eating, and increased time required to eat meals.
However, many patients adapt well to these changes, especially with proper support and gradual adjustment. The key factors for successful adaptation include:
- Comprehensive education about tracheostomy care and management
- Strong support systems from family, friends, and healthcare providers
- Access to appropriate communication aids such as speaking valves
- Professional counseling when needed to address emotional and psychological adjustment
Return to Normal Activities
Many patients successfully return to work, social activities, and hobbies after adapting to their tracheostomy. The timeline for returning to normal activities varies, but most patients can expect:
- Gradual increase in activities over the first few months
- Return to work for many patients, often with minor accommodations
- Participation in social events with proper planning and preparation
- Travel capabilities with appropriate supplies and medical clearance
Conclusion: Moving Forward with Confidence
A tracheostomy represents a significant medical intervention, but it doesn’t have to limit your life indefinitely. With proper education, support, and preparation, patients and families can successfully manage tracheostomy care and maintain a good quality of life.
The key takeaways for anyone facing a tracheostomy include:
Education is Essential: Understanding the procedure, care requirements, and potential complications empowers patients and caregivers to manage care confidently.
Support Systems Matter: Building strong relationships with healthcare providers, connecting with other tracheostomy patients, and maintaining family support systems significantly impact outcomes.
Financial Planning Helps: Understanding insurance coverage, exploring assistance programs, and budgeting for ongoing costs reduces financial stress and ensures access to necessary supplies.
Adaptation Takes Time: Allow yourself time to adjust to changes in communication, eating, and daily activities. Most patients find that life becomes more manageable as they develop confidence and routines.
Quality of Life is Achievable: While a tracheostomy brings challenges, many patients successfully return to fulfilling, active lives with proper support and care.
Remember that your healthcare team, including doctors, nurses, respiratory therapists, and speech-language pathologists, are valuable resources throughout your tracheostomy journey. Don’t hesitate to ask questions, seek clarification, or request additional support when needed.
The path forward may seem daunting initially, but thousands of patients and families successfully navigate life with a tracheostomy every day. With the right knowledge, preparation, and support, you can too. Focus on taking one day at a time, celebrating small victories, and building confidence in your ability to manage this new aspect of your healthcare journey.
Your strength and resilience, combined with medical advances in tracheostomy care, provide the foundation for moving forward with hope and determination. The medical community continues to improve techniques, equipment, and support systems to enhance outcomes and quality of life for tracheostomy patients, making the future brighter for everyone facing this journey.
Must Learn – Anatomy and Physiology of Nose: How We Breathe and Smell
Tracheostomy Procedure: A Comprehensive Guide on Tracheostomy Care Nursing Procedure
FAQs
1. What exactly is a tracheostomy?
Short answer: A surgical opening in the neck to insert a breathing tube directly into the trachea, bypassing the nose and mouth. It may be temporary or permanent.
2. How long will I need to keep my tracheostomy tube in?
Duration varies based on why the tube was placed. Some people have it for just days or weeks, while others need it long term. Stomas often close on their own after removal, leaving a small scar.
3. Will I be able to speak with a tracheostomy tube?
Speaking depends on tube type, cuff status, and vocal cord function. Many patients eventually resume speech using a Passy‑Muir speaking valve or speaking exercises guided by a speech‑language pathologist.
4. Is it safe to eat and drink with a tracheostomy?
Most patients can eat safely after proper swallowing assessment. Initial diets may require texture modifications like thickened liquids. A speech therapist helps guide the process to reduce aspiration risks.
5. What happens if the tracheostomy tube becomes blocked or falls out?
Blockage signs include labored breathing and inability to suction. First-line response: suction, saline flush; if unsuccessful, provide bag‑valve ventilation and seek medical help. Have a backup tube and emergency plan ready.
6. How should I keep my tracheostomy clean at home?
Clean the stoma daily with saline and gauze. Inner cannula cleaning typically every 8 hours or daily. Change ties weekly or as needed. Humidifiers or vaporizers should be used to maintain moist airways.
7. Why do I need a humidifier with a tracheostomy?
Because inhaled air bypasses the nasal passages, the lungs don’t receive natural moisture. Humidified air helps thin secretions and reduce airway irritation.
8. How long does recovery take after tracheostomy surgery?
Most healing happens within two weeks. Patients may need a few days to adjust to breathing via the tube, and sometimes up to a fortnight before day‑to‑day routines feel more natural.
9. Can I shower or bathe while having a tracheostomy?
Yes—with precautions. Use a shower shield and keep the neck angled back to prevent water entry. Sitting in water is okay as long as the stoma and tube stay dry.
10. Can I travel with a tracheostomy?
Yes. Be prepared: carry extra supplies (cannulas, suction catheters, saline, gloves, etc.), inform airlines of medical equipment, and consider insurance coverage. Equipment like suction machines may have restrictions onboard.
11. What are the most common complications of a tracheostomy?
Early complications: infection, bleeding, tube displacement. Later risks include tracheal stenosis, accidental decannulation, and tracheo‑arterial fistula, though major adverse events are rare with proper care.
If you have any questions or concerns, feel free to leave a comment below. We’re here to help and will do our best to provide you with the most accurate and helpful information.


I have not checked in here for a while as I thought it was getting boring, but the last several posts are great quality so I guess I’ll add you back to my daily bloglist. You deserve it my friend 🙂